Cardiac CT Scan: Advanced Chest Pain Investigation
New Technology Providing Early Detection of Heart Disease
In providing the most up-to-date care medical advancements provide, Dr. Zepick wants you to know that cardiac CT has come to the forefront in the investigation of chest pain and early detection of coronary artery disease.
New technology continues to be developed improve medical care and more effectively treat patients. Read on to understand how this advancement in cardiac medicine is giving cardiologists an enhanced view into seeing what is happening with a patient’s heart.

Image by Freepik
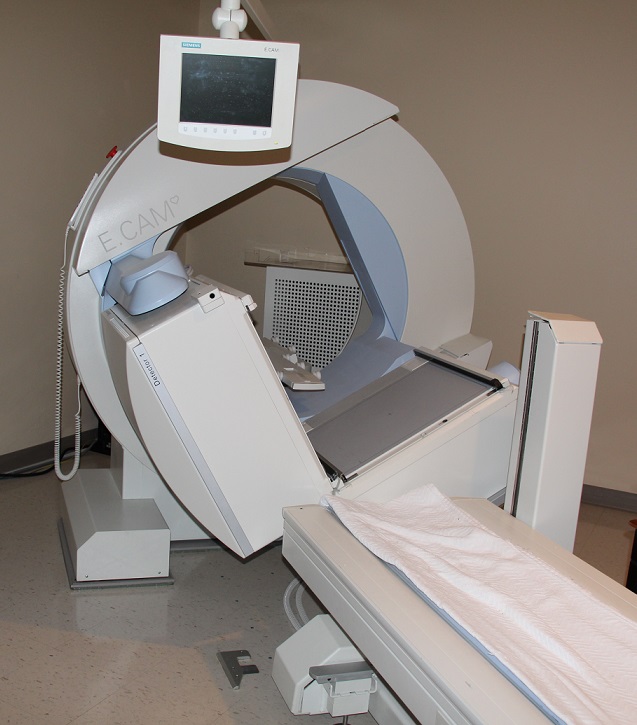
What is Cardiac CT?
Cardiac Computed Topography (CT) Scan is a procedure using x-rays to view the heart. With multiple x-ray beams, the scan records high-quality images from multiple angles to produce a 3D image of an individual’s heart. This image includes visuals of vessels and surrounding structures. Some of the areas shown in these CT scans include the coronary arteries, heart chambers, pulmonary veins, thoracic aorta and the pericardium, the sac around your heart.
Simply put, this is advanced technology providing cardiologists like those at Zepick Cardiology the clearest picture of your heart and surrounding areas. We’ve never had a better view of a person’s cardiovascular system.
When Does Someone Need a Cardiac CT?
A cardiac CT is used to look for a variety of cardiovascular issues, including:
- What could be causing chest pain or shortness of breath
- Source for blockages: potential calcium or plaque buildup
- Heart-related birth defects
- Tumors or masses around the heart
- Signs of aneurysms or problems with the aorta
Since these images provide such clear images of the heart and surrounding area, medical professionals are also utilizing these scans to help them prepare for procedures on their patients. The cardiovascular team may order a cardiac CT scan to prepare for a heart surgery or other procedures such as a transcatheter or an arrhythmia ablation.
Generally, a cardiologist orders a cardiac CT scan. However, the scan itself will most likely be performed by a team of trained technicians. Nurses will be involved to place an IV line or administer any necessary medications and doctors will oversee and interpret the images.

Image by Freepik
How Safe is the Cardiac CT Scan?
A cardiac CT scan is a relatively quick and low-risk procedure. In fact, the entire procedure usually takes between 30-60 minutes, and that includes preparation time. The actual scan takes less than 1 minute.
Because CT scanners use a small amount of radiation, they are not recommended for anyone who is pregnant, unless additional measures are taken to protect the baby.
You may receive medicine to slow down your heart rate for the scan. If you have asthma or COPD, that may impede normal breathing. Talk with your doctor if you have either of those conditions.
Preparing for a Cardiac CT Scan
While a cardiac CT scan is not invasive, it does require some preparation by the patient.
In advance of the appointment, consult with your healthcare provider on:
- All medicines you take, including over-the-counter.
- If you have diabetes, discuss how you may need to adjust your medications for the day of your test as you will be avoiding food for many hours.
- Inform them if you have any of these conditions:
- currently pregnant
- allergic to iodine, shellfish or any medications
- undergoing radiation therapy
- older than 60 or have a history of kidney problems
After a Cardiac CT Scan
After the scan is over, you will be released to go home. Then, you can go back to life as normal, enjoying your regular activities including eating, drinking, and taking your regular medicines (unless otherwise directed by your healthcare provider).
If you have diabetes or kidney disease, you may be instructed to increase your fluid intake to help get the iodine out of your body.
Getting your Scan Results
Your healthcare provider will inspect the images and interpret them. It will likely only take a couple of days before you come back in to go over the results.
More Information about Cardiac CT Scans
“Computed tomography coronary anatomy with functionality assessment could potentially become a first line in diagnosis.” Learn more about the state-of-the-art review of this advanced cardiological procedure in this article from the Journal of the American College of Cardiology.
For questions on cardiac CT scans or other heart issues, contact the experts at Zepick Cardiology in Wichita, Kansas. Call our office at (316) 616-2020.