How GLP-1A Weight Loss Drugs Like Ozempic Help Heart Health
Understanding Cardiovascular Effects of Diabetes Medications

There has been a lot of talk in the news about this supposed weight loss wonder drug called Ozempic. While this drug is primarily prescribed to help people with diabetes, what about people who suffer from cardiovascular problems? In this blog, we will explain the science behind this new medication and what effect it has on your heart health.
The first thing to understand is that Ozempic is just the brand name of one drug that provides these benefits. The active compound in drugs like Ozempic, Mounjaro, Wegovy, and Trulicity that has caused such great weight loss success in patients is something called GLP-1A.
Understanding GLP-1 Agonists
GLP-1A stands for glucagon-like peptide 1. GLP-1 agonists, like the active compound in drugs such as Ozempic, Wegovy, Mounjaro, and Trulicity, are a class of medications used mainly for managing Type 2 diabetes and obesity. These medications mimic the GLP-1 hormone which helps regulate blood sugar levels.
New in 2024: Weight Loss Drugs for People with Heart Disease

While the drugs primarily began being prescribed for the purposes of treating diabetes, now these drugs can be prescribed to patients to treat heart disease. In March 2024, the Food and Drug Administration (FDA) approved the active compound used in the brand name drug Wegovy® to be prescribed for cardiovascular care.
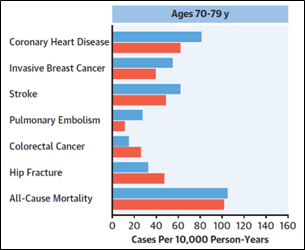
A study completed in late 2023 showed that medications with this compound, semaglutide, lowers certain people’s risk for heart attack and stroke by as much as 20%.
This FDA approval has allowed for heart disease patients to be diagnosed this medication if they are overweight and have cardiovascular disease. It is estimated that more than 6 million Americans fit this criteria.
Weight Loss and Its Impact on Heart Health
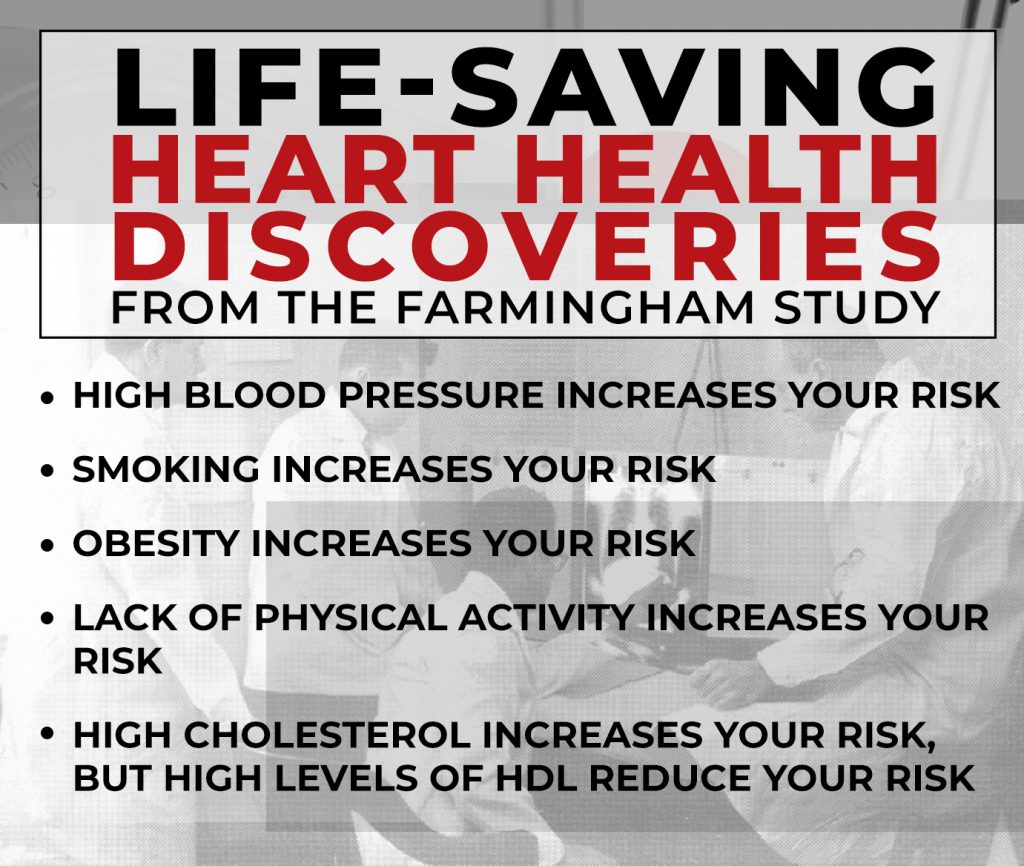
Obesity is closely linked to both heart disease and Type 2 diabetes. Excess weight increases the risk of high blood pressure, high cholesterol, and inflammation, all of which strain the heart and contribute to cardiovascular issues. Therefore, solutions to decreasing weight for those who are overweight also contribute to improving heart health.
How does Ozempic help your heart?
- GLP-1 agonists like Ozempic promote weight loss by slowing digestion and reducing appetite, leading to fewer calories consumed.
- This weight reduction helps lower cholesterol levels and blood pressure, reducing the strain on the heart.
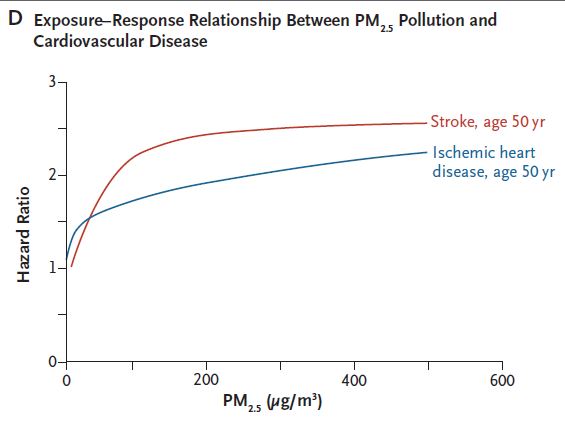
- Less strain on the heart decreases the likelihood of heart attacks, strokes, and other cardiovascular complications.
By addressing obesity, GLP-1 drugs support heart health, making them valuable tools for long-term cardiovascular care. At Zepick Cardiology, we emphasize the cardiovascular benefits of weight loss including the use of medication like those of GLP-1 agonists.
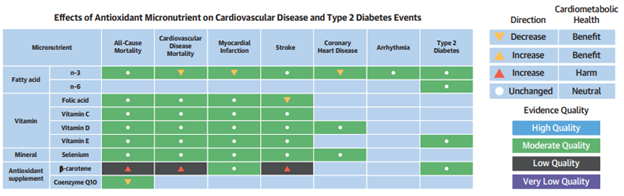
Recent studies show that these medications not only improve glucose control but also help protect the heart. They have been linked to reductions in cardiovascular events, such as heart attacks and strokes, particularly in patients with Type 2 diabetes.
By lowering blood pressure, improving lipid profiles, and promoting weight loss, GLP-1 agonists help reduce the overall risk of heart disease.
Wichita Cardiovascular Care
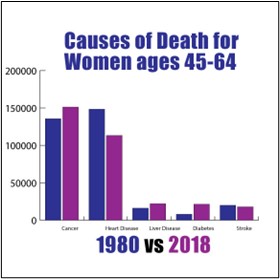
The findings of recent studies on weight loss drugs are significant for cardiology patients, as cardiovascular disease remains a leading cause of death in those with diabetes. Medications like Ozempic are becoming key components of comprehensive care, including addressing cardiovascular health.
For patients at Zepick Cardiology in Wichita, Kansas, we tailor treatment plans that may include GLP-1 agonists, improving not only diabetes management but also promoting long-term heart health.
Looking to see if you can be prescribed Ozempic or other weight loss drug? If you suffer with heart disease or other cardiovascular issue along with being overweight, contact Zepick Cardiology in Wichita to learn about your options.