11 Reasons to See a Cardiologist
Health Concerns & Symptoms for a Heart Specialist
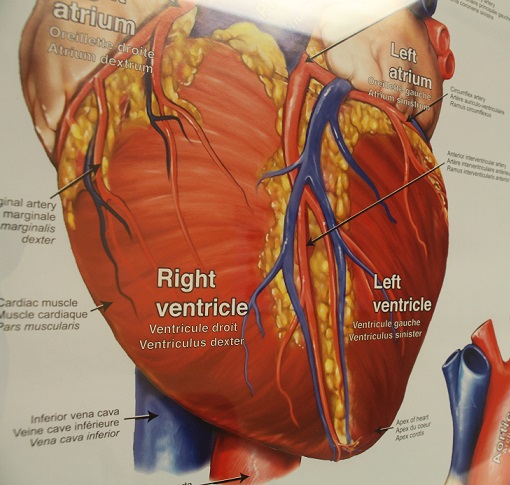
Simply put, a cardiologist is a specialist providing care specific to your heart health. While you receive the majority of care from your family doctors, a cardiologist in a cardiology clinic provides customized care necessary to look in depth at current or potential heart issues.
How do you know if it is necessary for you to see a cardiologist?
Let’s take a look at the common ways a person does see a cardiologist for the first time.
Often a person will first go to a cardiologist because they’ve been referred to see one by their primary doctor. If your doctor refers you to see one of our doctors at Zepick Cardiology or another Wichita cardiologist, do it. There would have been some reason to be concerned about your heart health for a doctor to make this recommendation.
The first times some people see a cardiologist is after a visit to the hospital. They came in with medical problems that indicate a potential heart issue.
But there are other times when it is prudent to make an appointment with a cardiologist.
When to See a Cardiologist
1. Family History of Heart Problems
Do you have a family history of cardiovascular issues? If your parents and/or grandparents had heart issues, there is good reason to worry about your own heart health. There is no guarantee you will have the same health problems they did, but there is an increased chance for it. Proactive measures are the best ways to keep your heart healthy and work to keep any hereditary issues at bay. A cardiologist can provide you with clear instructions for lifestyle change to help keep heart issues you may be genetically predisposed of at bay.
As you get older, inherited cardiovascular problems are likely to get worse. So, you don’t want to wait until the age your grandfather was when he had a heart attack. Getting checked by a cardiologist can give you the information you need early enough to work to prevent serious problems.
2. High Cholesterol
High cholesterol levels can lead to cardiovascular problems. What is quite dangerous about cholesterol problems is that they typically don’t cause symptoms. High cholesterol can be easy to ignore and yet also hard to manage. If you have discovered you have high cholesterol, it is best to take steps to lower your levels.
Diet and exercise go a long way in improving cholesterol levels. But sometimes a person’s cholesterol problems cannot be improved with either diet or exercise. A genetic or hereditary problem with cholesterol often requires medication to keep the bad cholesterol numbers low and to reduce your risk for potential heart problems. A cardiologist can work with you to create a heart-healthy plan as well as supply you with necessary prescriptions.
3. Smoking
If you’ve been smoking for a long time, you are at greater risk of having heart problems.
Quitting smoking can be an incredibly difficult habit to stop. Any medical professional will advise you to quit smoking, not just for your heart but for a variety of other health risks smoking causes. If you are not willing to quit smoking, do not let that stop you from seeking out medical care. Take the steps to speak with a cardiologist to learn what how your heart health may have been affected by a long history of smoking.
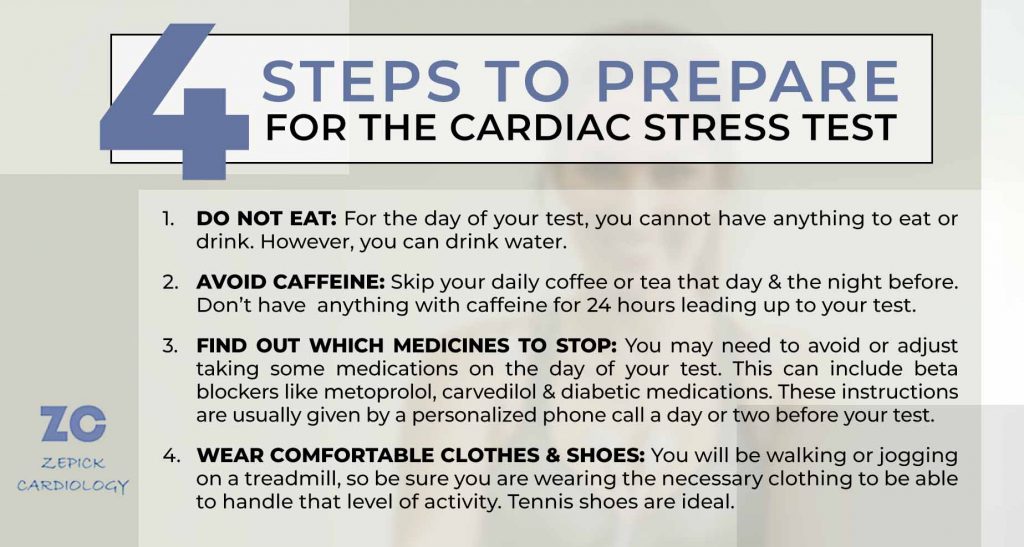
4. Embarking on a New Exercise Regimen
You’ve probably seen the warning given by workout programs to first consult with a doctor. This advice is given because starting a new exercise routine that may be difficult or strenuous and could increase your risk for heart or cardiac complications. Increased activity will, after all, put your heart to increased work.
Before starting a new exercise routine or regimen, it is advised that you speak with either your primary doctor or going right to a cardiologist for a heart check-up.
There have been new guidelines regarding medical checks before enhanced activity to help you know if you should seek prior medical advice. According to Penn Medicine, here are 3 questions to ask yourself before you start a new workout practice:
- Are you typically not active? If you mostly have a sedentary lifestyle, you may want to consult a doctor before you start a new exercise program.
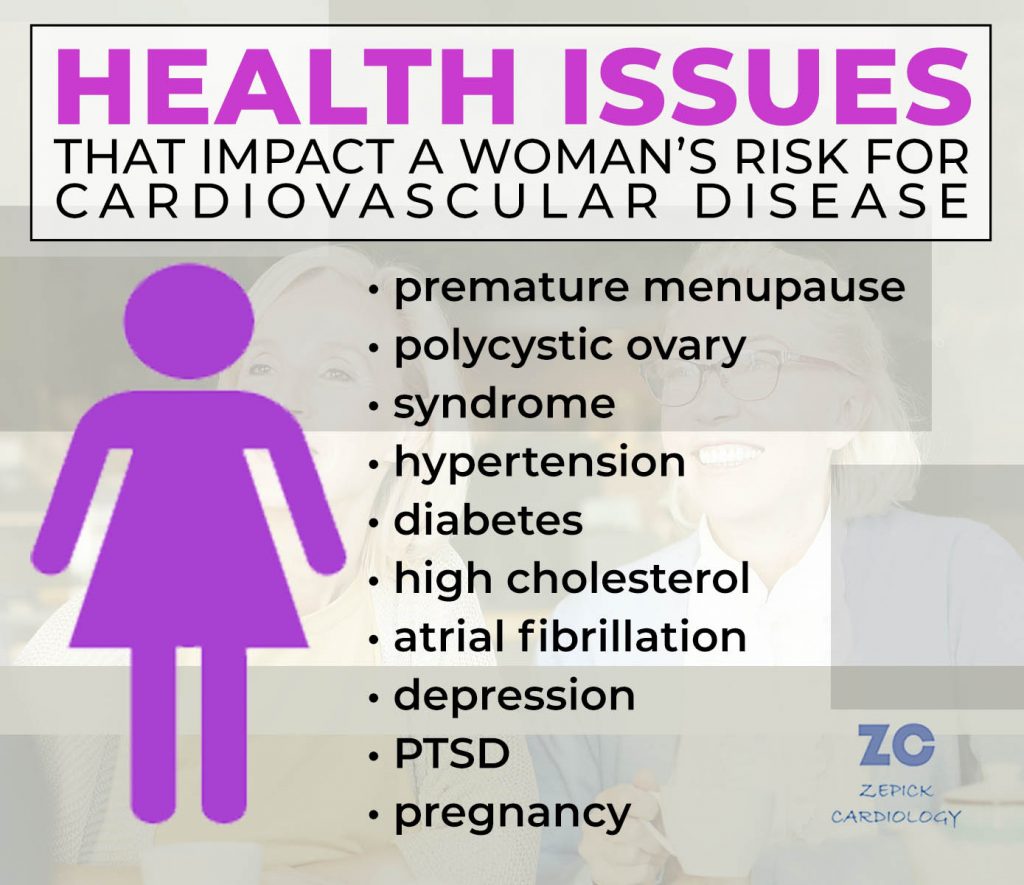
- Do you have signs of heart problems or other conditions that might put you at higher risk for having heart problems? Diabetes, kidney disease and lung disease are just some issues that can predispose you to heart issues. Consult this exhaustive list of conditions that put women at higher risk for cardiovascular problems.
- What is the exercise or activity you plan to participate in? If you are looking into starting a high-intensity exercise program (like running), you might want to visit a general doctor or cardiologist first. This is particularly true if you answered yes to the first question that you do not live a typically active lifestyle.
5. Gum Disease
Gum disease has been linked to heart problems. Bacteria from your gums can travel to your heart and lead to infections in your heart valves and inflammation in heart vessels. If you’ve been diagnosed with gum disease, you should visit with a cardiologist to make sure your heart health is in check.
Symptoms That May Indicate Cardiac Issues
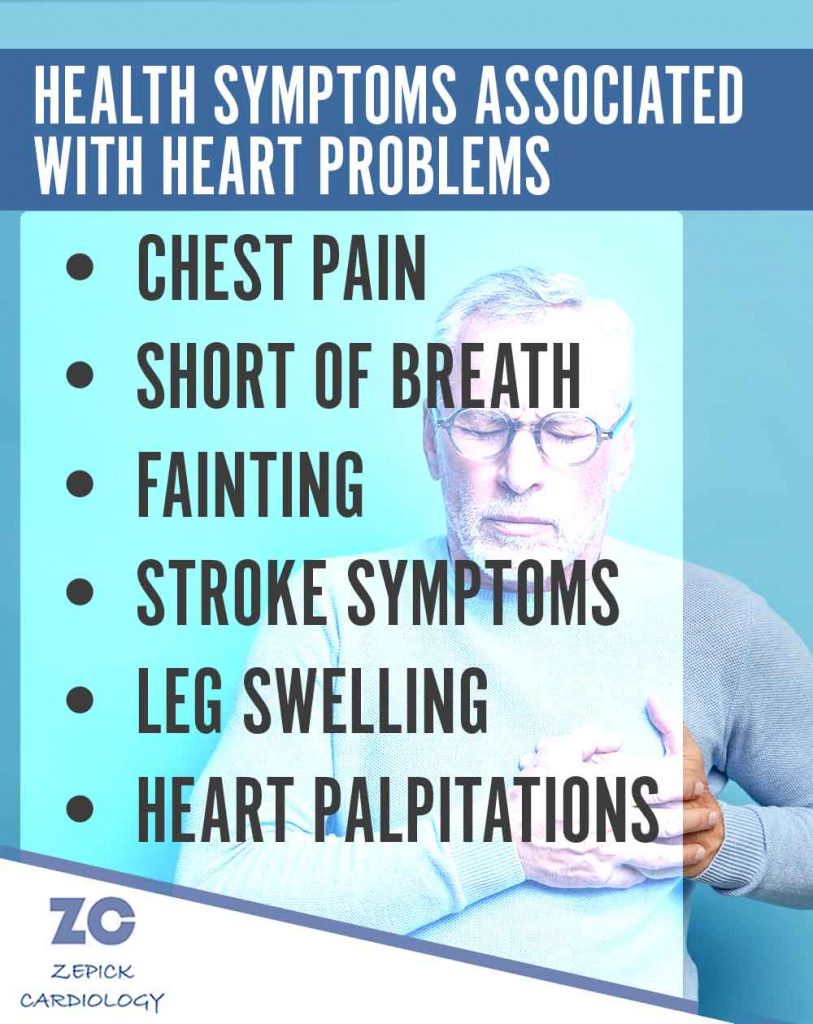
These next 6 reasons that lead to some people scheduling a visit with a cardiologist are because of certain physical ailments. These symptoms are often associated with cardiovascular issues. People who experience one or more of these could have serious heart problems that need to be diagnosed by a cardiologist.
6. Chest Pain
Chest pain, also called angina, is a real cause for concern. This could indicate a lot of serious health problems, including a heart attack or other cardiac issues.
There are many minor health issues that can cause chest pain, so feeling chest pain does not always mean that you are having heart problems. But because it is such a common ailment with someone suffering serious heart problems, it is a symptom that should not to be ignored or minimized.
7. Shortness of Breath
Feeling short of breath, like having chest pain, can mean a variety of different problems, some serious and some relatively minor. Shortness of breath, also called dyspnea, can indicate heart failure or other type of heart disease. For that reason, it is a symptom that may lead you to see a cardiologist.
When should you be concerned? Shortness of breath is a common, normal phenomenon when doing something strenuous or being in a high altitude, but if you experience shortness of breath that is not associated with extra physical activity, high altitude or weather changes, that symptom could indicate a health problem, potentially a life-threatening one.
8. Fainting
While many of us can recall an instance where we have passed out, that does not mean it’s an insignificant symptom that should be ignored. Fainting or passing out can be caused by an irregular heartbeat, which is called an arrhythmia. An arrhythmia occurs when there is a problem with the signals that control your heartbeat.
Diagnosing an arrhythmia isn’t simple, therefore it often requires an experienced cardiologist like those at Zepick Cardiology in Wichita. When getting tested, you may be asked about the circumstances surrounding your fainting spell including what you were doing, what and when you’d last eaten, and if you have any history of passing out.
9. Stroke symptoms (slurred speech, drooping face, numbness)
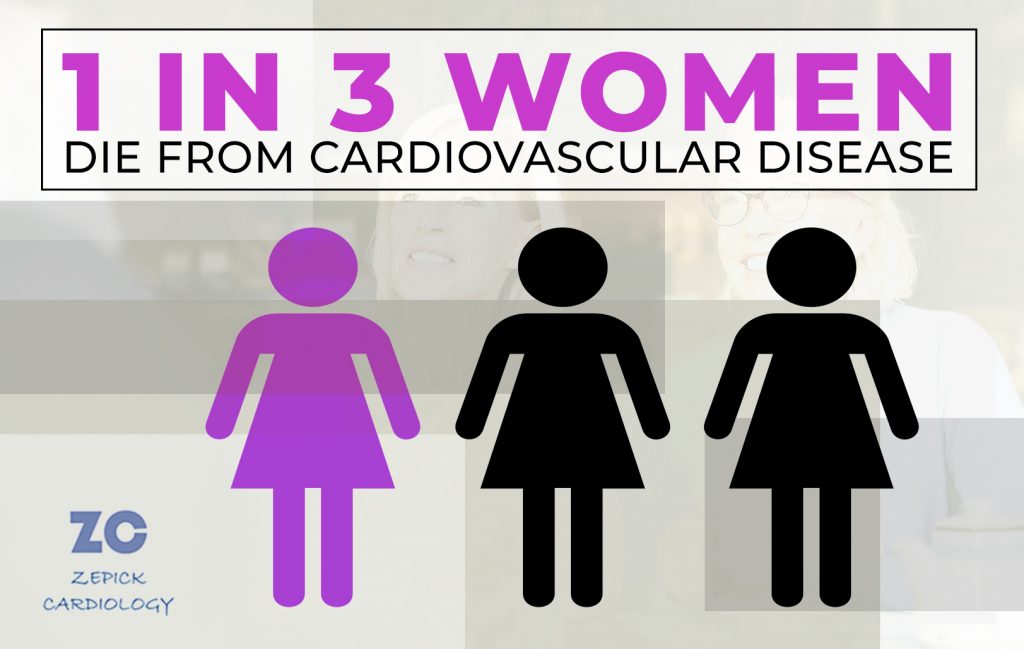
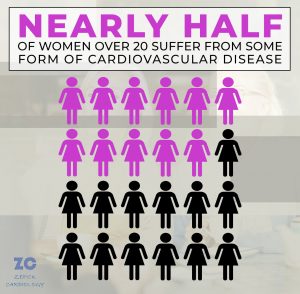
While cardiovascular disease is the number one cause of death among adults in the United States, stroke is the second. A stroke is when there is a problem keeping blood to get to the brain.
Are you aware of the acronym to help you quickly detect signs of a stroke?
F – Facial drooping
A – Arm weakness
S – Speech difficulties
T – Time to call 911
These symptoms are key to taking quick action for a person likely experiencing a stroke.
People with heart disease can have an increased risk for stroke. According to the National Library of Medicine, “9 out of 10 strokes can be prevented by controlling CVD (cardiovascular disease) risk factors.”
Issues with your heart such as high blood pressure can put you at greater risk for having a stroke. Getting any cardiovascular problems under control with the expert care of a cardiologist can not only help you prevent heart problems, but strokes as well.
10. Leg swelling

The issue of having ongoing swollen legs from excess fluid is called edema. It is often a sign of a heart problem.
When your heart isn’t accurately pumping blood through your body, the blood can back up in the veins in your legs. You may feel a pain, ache or burning in the muscles of your lower legs or feet. Sometimes these pains can show up during a walk then go away after resting for a few minutes. You may also feel too tired or weak to handle your normal day-to-day activities.
Having problems with swollen legs may be a clear indication that you should seek medical attention from a cardiologist to address your heart and blood flow.
11. Palpitations (skipping heartbeats)
Do you feel your heart fluttering? Is it pounding? Does it seem to be beating fast or even skipping beats? Having heart palpitations can be disconcerting as it can indicate serious problems with your cardiovascular system.
There are several factors that can cause heart palpitations other than heart disease, including some medications and exercise. A fever may cause palpations, as can depression or having too much coffee. Many people feel these sorts of heart irregularities for rather harmless reasons.
But there are times when this symptom indicates a more serious heart problem. If it’s happening frequently and lasting for longer than a few seconds, it could be from an issue that should be evaluated by a heart expert. This is especially true if it is accommodated by such other symptoms as fainting, chest pain, shortness of breath or dizziness.
What should you do if you fit into one of those categories?
One thing you can do if you have any of these concerns is to consult with your regular doctor. You should expect a doctor to listen to your concerns and provide you with some information and advice on next steps. They may refer you to a cardiologist for further medical testing.
You can also make an appointment with a cardiologist directly. To contact Zepick Cardiology here in Wichita, call (316) 616-2020. Even without a doctor’s referral, you can make arrangements to visit with a heart specialist on the health concerns you have.